Sacral Ulcers

Sacral ulcers are a painful and potentially dangerous type of skin lesion most often experienced by nursing home residents who are not receiving proper preventative care. Left untreated, ulcers can lead to serious skin decomposition, infection, sepsis and even death.
Sacral ulcers in nursing homes are preventable. If you or a loved one have suffered a sacral ulcer due to nursing home neglect, you may be eligible to receive compensation for your medical bills, pain and suffering and more. Learn more about your rights and possible options by contacting a nursing home abuse lawyer.
Call Fight Nursing Home Abuse at 1-866-548-9636.
What Are Sacral Ulcers?
A sacral ulcer is a type of pressure injury (also called a decubitus ulcer or bedsore) caused by lengthy periods of direct pressure over a bony area of the body. These wounds are often a sign of nursing home abuse or nursing home neglect.
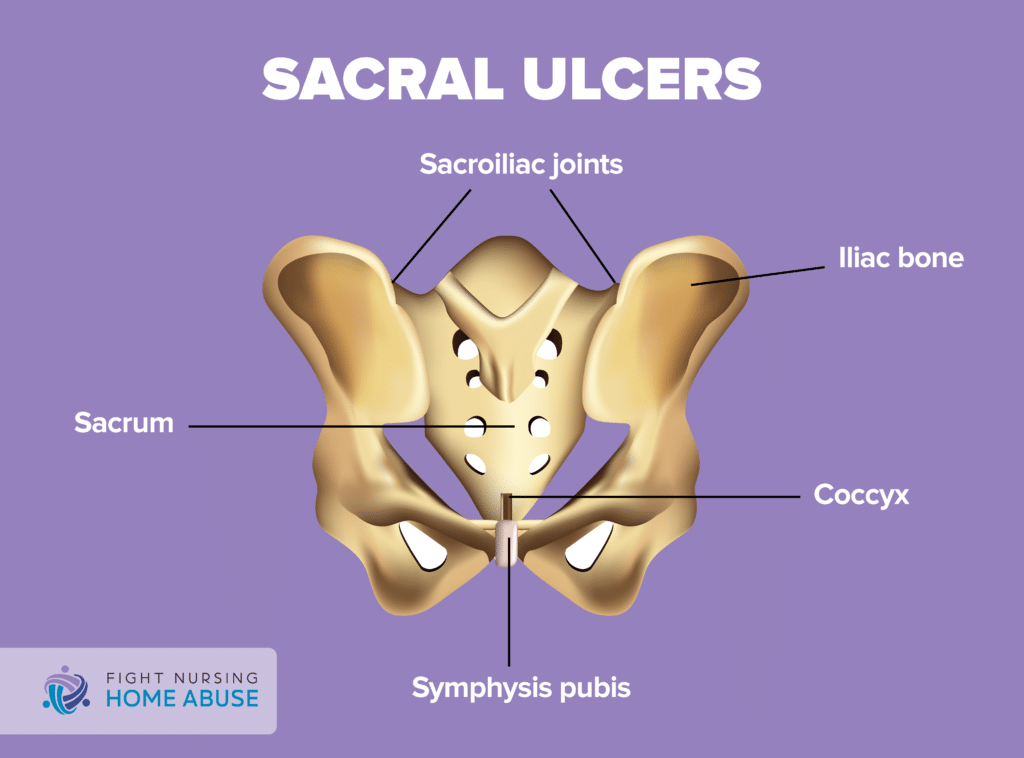
The sacral region of the body lies between the L5 segment of the lumbar spine and the coccyx (tailbone). This area is comprised of five segments that are fused together to create a triangular shape. The sacrum is also the back wall of the pelvis and joins at the hip bone (sacroiliac joints).
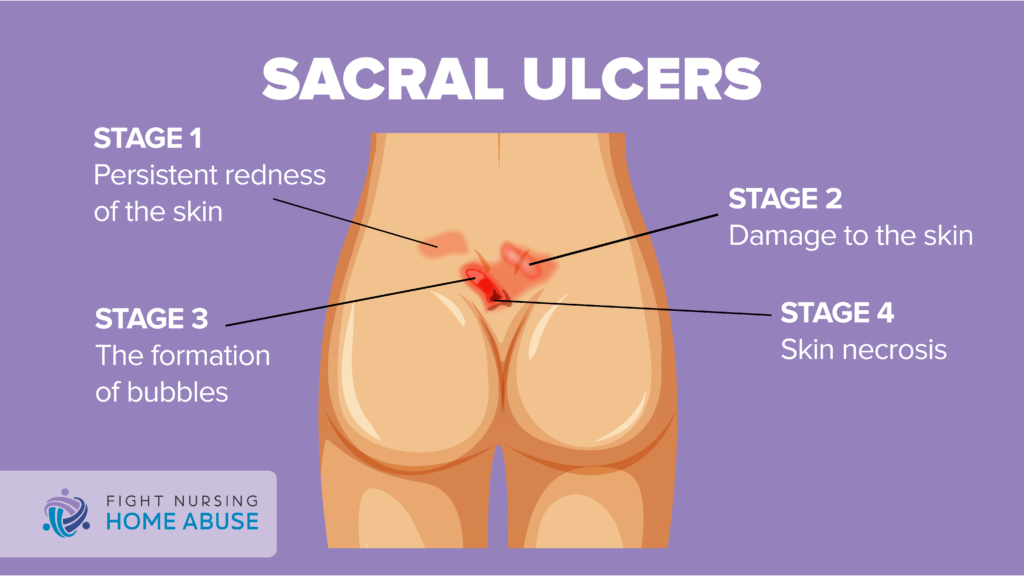
Direct pressure such as that applied by the weight of a body lying prone in a nursing home bed interferes with the blood supply to the area. Resulting skin decomposition creates a wound that at first may appear as a blistered area over the sacrum. As the sacral ulcer worsens, it opens into a crater-like wound.
It is critical that sacral ulcers are treated immediately.
How to Recognize a Sacral Ulcer
Any nursing home resident who complains of lower back pain should be examined immediately to rule out a sacral ulcer. Staff must monitor residents who are incapable of self-reporting pain regularly during bathing, clothing changes, toileting and other hygiene activities.
Seek medical attention for the resident if you notice any of the following in the sacral area:
- Unusual changes in skin color, texture, or temperature
- Pus-like draining
- Skin that is tender to the touch
- Swelling
- Blistering or an open wound
Treating Sacral Ulcers
A sacral ulcer is a type of pressure ulcer – also called a decubitus ulcer, pressure sore, or bedsore. It is a wound that is located in the sacral area. Treating these wounds follows similar guidelines to treating pressure ulcers. Treatment options often include:
Reducing Pressure
Repositioning the patient regularly to prevent pressure points and reduce friction is one of the best ways to prevent worsening or development of new pressure ulcers. Also, using support surfaces like mattresses or cushions can provide support and protect the skin.
Wound Care
Proper wound care is essential for treating pressure injuries anywhere on the body. Pressure ulcers begin as a wound, but without proper care, they quickly worsen and there is damage or death to affected tissues. Wound care should come from a doctor or nurse who specializes in wound care and who has experience managing pressure ulcers.
Removing Tissue
When skin and bodily tissue has damage or dies, it can become dangerous to surrounding tissues. Healthcare providers can remove this tissue through a process called debridement. The wound is washed thoroughly and damaged or dead tissue is cut away. It is important for wound healing that appropriate dressings are used to keep bacteria out and reduce the risk of infection.
Negative Pressure Wound Therapy
Negative pressure wound therapy, or NPWT, is a process that draws out fluid and infection from a wound. Then, a special bandage (dressing) is applied, which seals the wound. Finally, a special vacuum pump is attached, which draws out air and fluid, and prevents infection. This method also allows antibiotics and saline solution to be applied directly to the wound without having to exposure the area.
Medications
Medications are often a part of treatment for pressure ulcers, including those in the sacral region. Medication treatments often include:
- Nonsteroidal anti-inflammatory drugs (ibuprofen, Advil, etc.)
- Pain relievers (Naproxen sodium, Tylenol, etc.)
- Topical pain relievers
Surgery
Sometimes pressure ulcers are so severe that they require surgery. Surgery done to treat these wounds often includes skin grafts or repair to the deeper tissues, including the muscle. Surgery may also include using skin, muscle or other tissues to pad the affected area, especially if tendons and bones are showing.
What Are the Risks of a Sacral Ulcer?
Sacral ulcers can quickly become a serious medical concern. Prompt medical care and ongoing preventative measures are necessary to limit the damage and prevent recurrence. If left untreated, these injuries can cause:
- Cellulitis, a painful skin and connective tissue infection
- Bone and joint infections such as septic arthritis or osteomyelitis
- Squamous cell carcinoma, a type of cancer caused by wounds that do not heal
- Sepsis and septic shock, a dangerous and potentially fatal condition
Who is Most At Risk in Nursing Homes?
Nursing home residents are more at risk of developing a sacral ulcer than the general public. Within the nursing home, the patients most at risk include:
Residents with Limited Mobility
Nursing home residents with limited mobility, or who are immobile, are most at risk for pressure ulcers. Particularly at risk are those who are confined to bed.
Residents with Medical Conditions
Nursing home residents with medical conditions are more at risk for pressure sores. Diabetes or a vascular disease are particularly concerning as reduced or interrupted blood flow increases the risk of tissue damage. Conditions that cause urinary or fecal incontinence also increase the risk. Both conditions create a moist atmosphere in which sacral ulcers flourish and introduce bacteria to the ulcer.
Residents with Sensory Issues
Lack of sensory perception, as a loss of sensation can result in a lack of awareness of pain that would otherwise tell the resident to change positions. This raises the risk of developing a pressure ulcer due to constant sacral pressure. Inability to identify pain or discomfort can lead to unrecognized shearing forces, meaning that the skin is moving in two different directions. Without assistance, friction and shear can quickly lead to pressure ulcer development.
Inadequate Nutrition
Malnutrition and/or dehydration are both risk factors for pressure ulcers. Lack of adequate nutrition means the body does not receive enough fluid and nutrients to maintain healthy skin and prevent tissue breakdown. It also makes the resident’s overall health compromised, which can make medical conditions worse.
How Can You Prevent Sacral Ulcers?
Rigorous, proactive preventative care is the key to preventing sacral ulcers in nursing homes. Nursing home staff must have the training, time and tools necessary to carry out personal care and hygiene activities including:
- Frequent repositioning to avoid constant pressure on one area of the body
- Specialty beds or wheelchairs that tilt to facilitate more frequent pressure changes
- Frequent cleansing of the area with a gentle soap and thorough pat dry, to remove moisture and bacteria
- Regular clothing/bedding changes and laundering
- Daily skin inspections and skin care
- Adequate and nutritious meals
- Suitable products for incontinence, with frequent changes and cleansing
- Barrier cream, where fecal incontinence makes wound sanitation difficult
- Sacral dressing, to protect the area and encourage healing
Caregiver vigilance is the most critical factor in preventing sacral ulcers in nursing homes. If you suspect that nursing home abuse or neglect has resulted in a sacral ulcer, help is available.
How Much Compensation is Available for Sacral Ulcer Sufferers?
In cases of nursing home abuse or neglect, compensation can cover medical treatment, personal care services, and therapies. It can also compensate the victim for pain and suffering.
If you have lost a loved one due to nursing home neglect, there may be compensation to pay for:
- Medical expenses before death
- Funeral and/or burial costs
- Suffering experienced before passing
Call Fight Nursing Home Abuse to learn more. Nursing abuse lawyers have the experience and resources necessary to deal with nursing home neglect complaints. A lawyer will pursue justice and compensation from all liable parties, including securing all available compensation from applicable insurers. Where that is not possible, they will fight for your rights in court.
How to Get Help if You Suspect Nursing Home Abuse or Neglect
Call 1-866-548-9636 to learn more and schedule your free consultation.


