Bedsores
Bedsores, also known as pressure sores, decubitus ulcers and pressure ulcers, are one of the many signs of nursing home abuse, nursing home neglect, or medical malpractice in a hospital. Bedsores develop when there is unrelieved pressure to the skin on a certain part of the body. These injuries can cause serious health problems like infections, sepsis and other life-threatening injuries.
Bedsores occur most frequently to areas of the body where bone and skin are very close in contact, such as the hips, back, elbows, ankles and heels. Nursing home residents and people staying at a hospital are at high risk for bedsores or pressure ulcers because they often times remain sedentary in a bed or wheelchair.
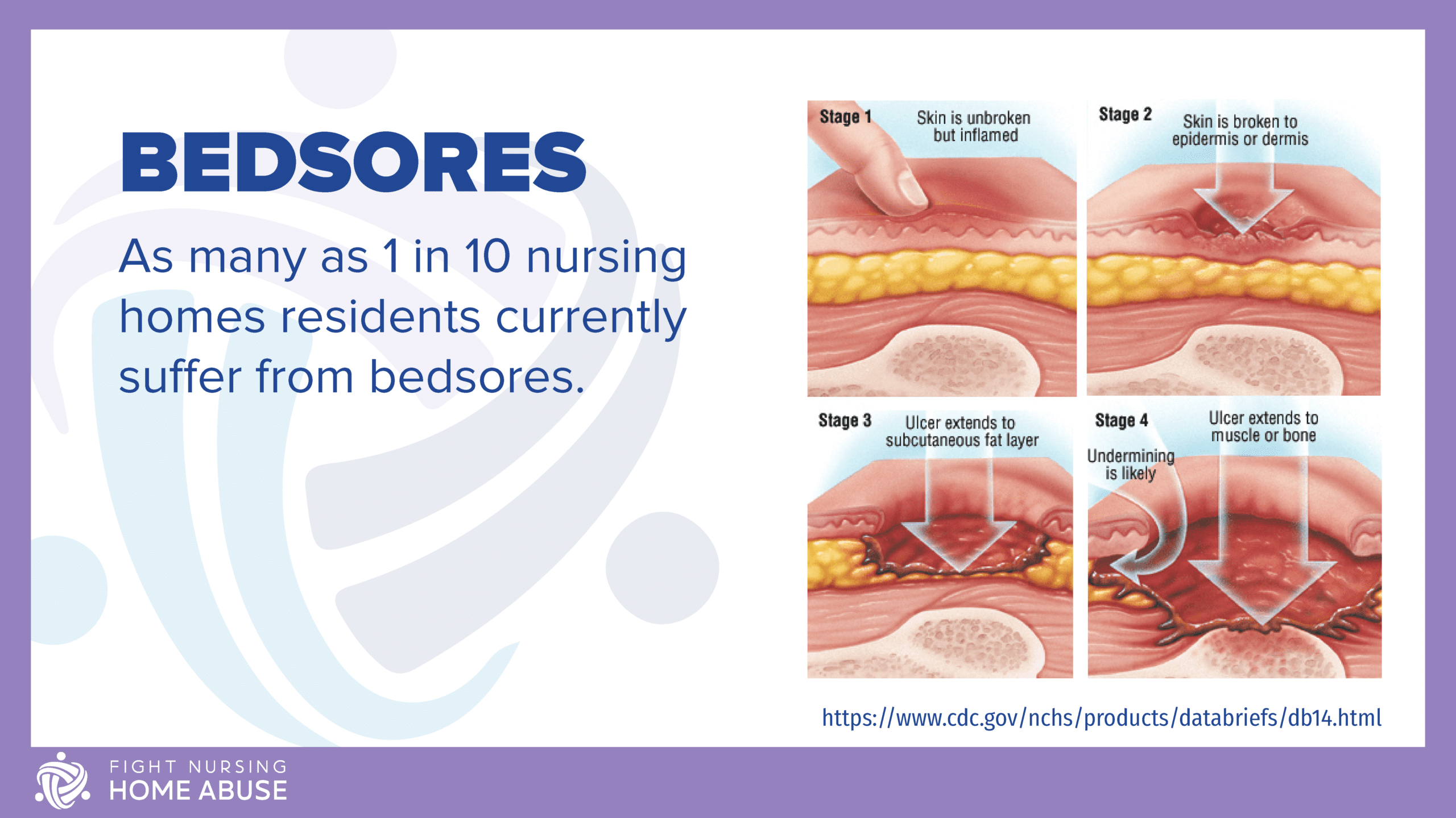
According to the Centers for Disease Control and Prevention (CDC), as many as one out of 10 nursing home residents currently suffer from bedsores. Although this is alarming to many, this isn’t a new problem. For several decades, bedsores have been a prevalent problem in nursing homes throughout the United States. In many instances, bedsores are caused primarily from lack of attention and improper medical care in nursing homes.
What are Bedsores?
Bedsores are wounds that develop when blood supply to the skin is cut off for more than 2-3 hours. The technical term is ‘decubitus ulcers’, but most people call them bedsores. What begins as inflammation quickly progresses to skin death. Eventually, the wound turns purple and the skin can break open. Without immediate treatment, a bedsore can worsen, going deep into tissue, muscle and bone.
Individuals who have bedsores are at a high risk for infection, and may experience a long recovery time of up to months or years. Recovery time will depend on the severity of the injury, or stage.
Stages of Bedsores
Hospitals and nursing homes use a scale to help determine the severity of bedsores. By using this scale to categorize bedsores according to their typical characteristics some uniformity can be established. This assists medical facilities in the treatment of those suffering with bedsores. Bedsores are staged in 4 stages, with 1 being the least severe and 4 being the most severe.
Stage 1 Bedsore
At first, a bedsore will appear as an area of skin that is red and possibly itchy. This area may also feel firm or warm and spongy to the touch. People with darker skin may have an area with a purple or blue hue, rather than the aforementioned red. It could also look ashen or flaky. Stage 1 bedsores will generally heal once the pressure has been relieved.
Stage 2 Bedsore
Some skin loss has occurred at this point and the sore may appear as an open wound. Skin loss can be in the epidermis, which is the outer layer of skin or in the dermis, which is the deeper layer of skin. Some sores also affect both of these layers. The wound has become a sore that resembles an abrasion or blister. The tissues surrounding it may have a purple or red discoloration. If this bedsore is treated promptly, these injuries generally heal rather quickly.
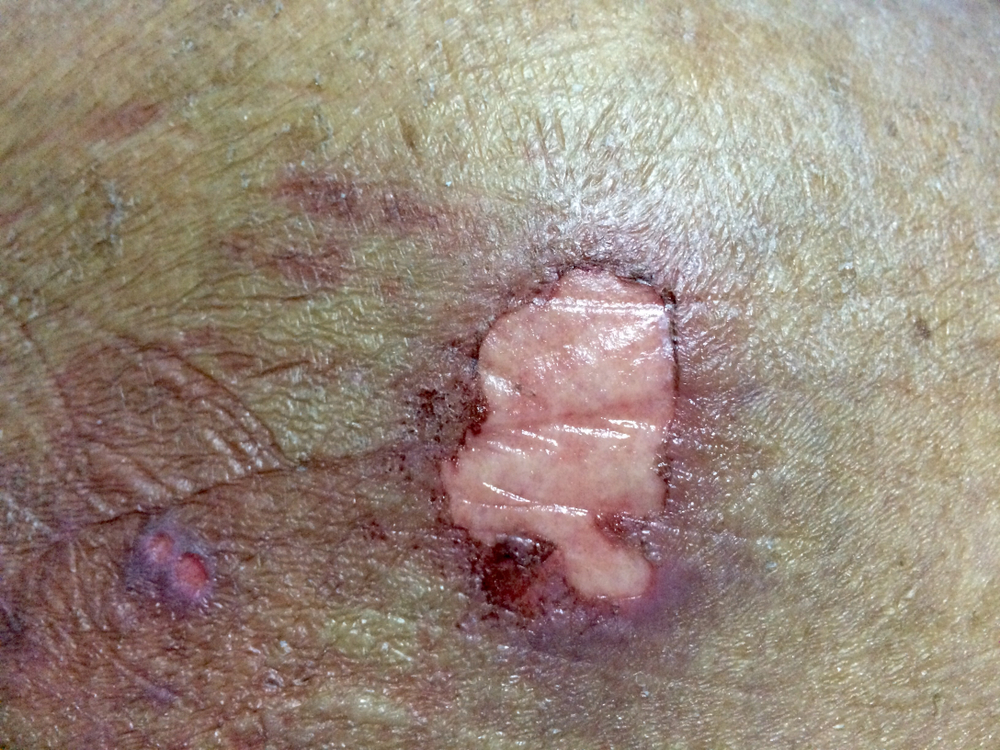
Stage 3 Bedsore
Once the bedsore reaches this stage, all layers of skin have been affected down to the muscle. This process damages or destroys tissue. The wound is now deep, resembling a crater (known as slough). The open skin may show fat around the infected area. At this stage, treatment is crucial to preserving tissue, removing dead tissue and preventing infection.
Stage 4 Bedsore
This is the most advanced and serious stage. Damage has now been done to the bone, muscle and the joints and tendons, which are the supporting structures. Large amounts of skin have been destroyed and these wounds are very difficult to cure. At this stage, dead tissue can lead to lethal infections. Stage 4 bedsores can be life-threatening, so timely treatment is essential. In many cases, surgery is required to remove tissue. Sometimes surgeons must amputate an affected limb to remove dead tissue and prevent sepsis or gangrene.
Unstageable
On occasion, a bedsore will be categorized as ‘unstageable.’ These are generally extremely advanced wounds involving muscle, skin and bone (full-thickness tissue loss). Unstageable bedsores are deep and are covered in “slough” or “eschar”. Slough is generally tan, gray, green or brown. Eschar is generally tan, black or brown. These deep wounds also often have a foul odor and may ooze pus and fluid.
Bedsore Treatment
There are a few ways to treat bedsores, which depend upon the stage of the wound and other factors like the presence of infection. For stage 1 sores, a combination of antibiotics and cleaning solutions are usually effective. Treating pressure sores also requires repositioning regularly. Supportive aids should always be available, such as specialized cushions, pillows and mattresses.
For advanced stages, victims may need to undergo surgery via mechanical, autolytic or enzymatic debridement in order to successfully remove the damaged tissue. Afterwards, cleansing and bandaging the wounds is extremely imperative and must be done regularly. Pain medication and antibiotics are typically prescribed as well.
Along with pain medication and antibiotics, pressure ulcer patients should eat a healthy diet. Nutrition and hydration will help the healing process. In addition, muscle relaxants may be prescribed as some victims experience muscle spasms as they heal.
Tips for Bedsore Prevention
Bedsores are a tragic sign of neglect. It is best to prevent bedsores before they start. Too often, however, bedsores are already at an advanced stage before being noticed, which in turn requires long and difficult treatments. In order to help prevent pressure injuries, a number of activities can be done to ensure the best possible chances.
Change positions regularly
People with limited mobility should change positions every 15 minutes to relieve pressure. Patients who are confined to a hospital bed should change positions at least every two hours. It also helps to avoid laying directly on the hip bones. Instead, patients should lay at a 30 degree angle to reduce pressure on the hips. Patients should not have their head raised more than 30 degrees, as this encourages the body to slip down and raises the risk of friction injuries. Pressure-reducing mattresses can relieve pressure and be helpful in reducing pressure ulcers.
Inspect skin daily
Inspecting the skin is a great prevention tool to incorporate into any daily care routine. Caregivers in nursing homes should inspect skin daily, especially when assisting with bathing or other hygiene. Also, skin should be kept clean and dry. If the patient has bandages, it’s imperative to make sure they are changed daily. If there is skin damage, foul smell, infection or tenderness or changes in skin color, you should seek medical attention immediately. Skin care is one of the top ways to prevent bedsores.
Pay close attention to nutrition
Malnutrition can lead to bedsores as well as other diseases and illnesses. It is essential to get enough calories, protein, fat, vitamins and minerals. Nursing homes should consult a dietitian to come up with eating plans for residents that appeal to their food preferences while also supplying the necessary nutrients. Residents who cannot feed themselves or who have special dietary restrictions should be provided with assistance to make sure they are getting adequate nutrition and hydration throughout the day.
Try to exercise every day
Exercising increases blood flow throughout the body, which aids your skin care regimen. It also promotes a positive mood and socialization. Each of these is important for nursing home residents. Caregivers should consult with a physical therapist for exercise programs that are beneficial to patients. Routine and safe exercise can help improve overall health and wellbeing, which in turn can help prevent bedsores and other illnesses or injuries.
Common Areas to Monitor for Bedsores
Depending upon the circumstances, bedsores will manifest on different areas of the body. For example, a person who is confined to a wheelchair will have different areas of the body affected as opposed to someone who is confined to a bed. Caregivers should monitor residents based on their mobility levels and overall health.
Residents in Wheelchairs
For residents in wheelchairs, caregivers should routinely assess:
- The buttocks area and/or the tailbone.
- The back both the legs and arms, in the areas that these body parts rest for long periods of time against the wheelchair.
- The spine and/or the shoulder blades.
Residents Confined to Beds
Residents who are confined to a bed should be routinely assessed for skin health in the following locations:
- Both sides and the back of the head
- The outside areas of the ears, specifically on the rims
- Shoulders and shoulder blades
- Lower back and hips
- Knees, heels, and ankles
Most bedsores are the result of friction, shear and sustained pressure. That’s why they are also called pressure ulcers and pressure sores. Residents, especially those confined to a wheelchair or bed, should be assessed regularly even if their positions are moved frequently.
Medical Complications as a Result of Bedsores
Bedsores can lead to an array of other medical conditions if not monitored and treated in the early stages. Proper wound care is essential for healing and preventing complications. Some possible complications include:
- Cancer: Chronic sores can develop into squamous cell carcinoma, a destructive type of cancer that almost always requires surgery.
- Joint/Bone Infections: Bone and joint infections develop after burying themselves deep into pressure sores. Also known as infectious or septic arthritis, these types of infections can not only damage cartilage and tissue, but can also severely restrict joint functions.
- Sepsis: Sepsis occurs when bacteria enters into the victim’s bloodstream via the open pressure sores. Instead of fighting off the bacteria, the body turns on itself. Sepsis can quickly spread throughout the body resulting in life-threatening organ failure and other issues.
- Cellulitis: Cellulitis, an inflammation of connective tissues, can also infect victims of bedsores. If cellulitis occurs, victims may develop meningitis, which affects the fluid that surrounds the spinal cord and brain.
Prognosis for Patients with Bedsores
The prognosis for a patient with a bedsore or pressure ulcer depends on the stage of the sore and other factors. If the bedsore is diagnosed and treated quickly, the prognosis is generally favorable. Recovery may take only a few days or weeks. Patients with a more severe bedsore, infection or sepsis may experience a much longer recovery period. Sometimes, it can take weeks or months for a sore to heal. If the wound requires surgery or amputation, the recovery period is much longer.
Patients with bedsores often also experience long-term pain, depression and social isolation. Part of improving the patient’s prognosis is making sure that he or she has access to adequate nutrition, hydration, exercise, social interaction and medical care. Healthy skin is a critical part of preventing bedsores (pressure ulcers or pressure sores).
Getting Help with Bedsores
If you suspect your loved one has a bedsore, pressure ulcer, or pressure sore – you may have questions and concerns about their care and how to help them. At Fight Nursing Home Abuse, we can help. Our team of nursing home abuse lawyers and advocates know how difficult it is to consider that your loved one has been abused or neglected. We are dedicated to helping nursing home residents and their families protect their rights and their wellbeing.
If your loved one has been diagnosed with a bedsore, pressure ulcer, decubitus ulcer, or pressure sore – contact us to find out how we can help. A free consultation with one of our lawyers will help you get started protecting your loved one. Whether you have questions about wound care, your loved one’s legal rights, or want to report abuse or neglect – we can help.


