COVID-19: A Global Crisis in Nursing Homes Continues
Long before the novel coronavirus COVID-19 was on the radar, health officials warned that nursing homes were vulnerable. Many believe that those warnings fell on deaf ears. As coronavirus in nursing homes has spread, facilities continue to experience gaps in infection control and efforts to prevent viral outbreaks.
Once COVID-19 started to spread in nursing homes, the extent of those vulnerabilities became all too clear. Across the world, nursing homes continue to be the hardest hit population. In the United States, 40% of COVID-19 deaths have occurred in these facilities.

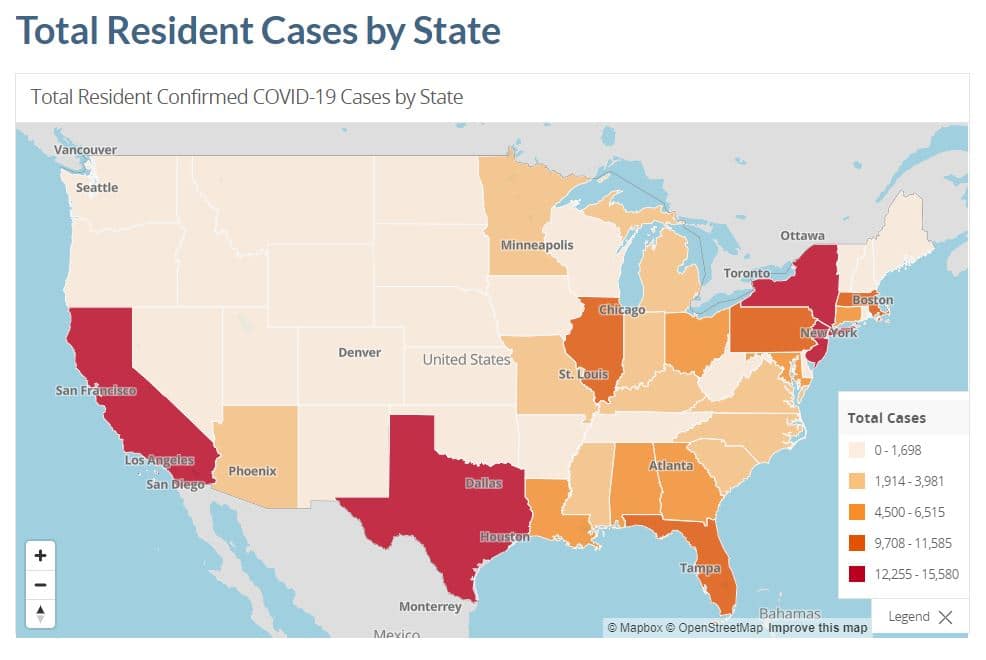
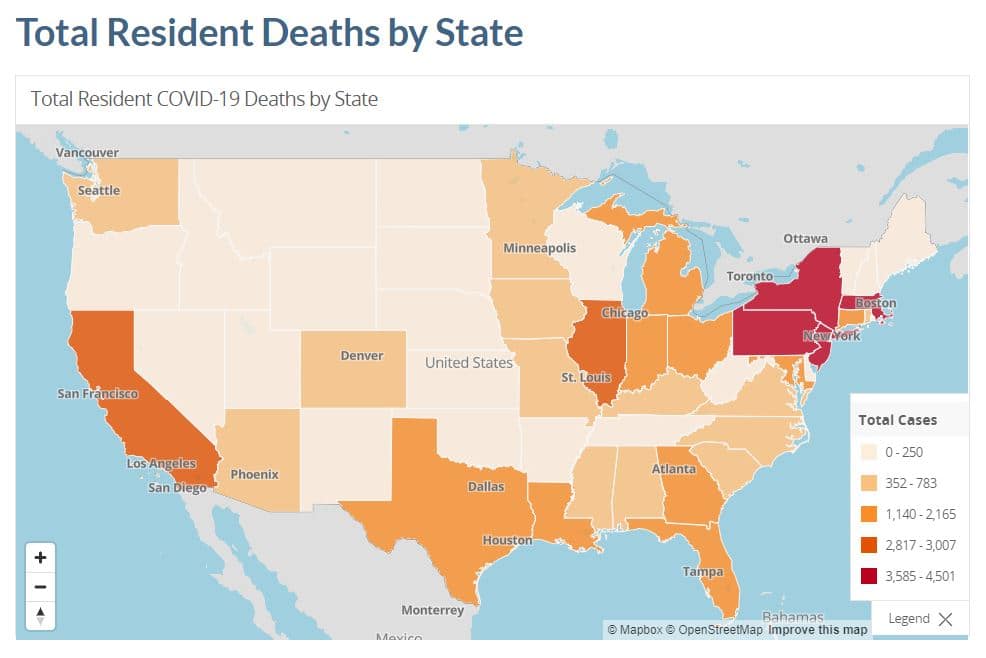
Experts say that the number of COVID-19 deaths in U.S. nursing homes is on the decline, but rates of positive cases are still climbing in some states. Overall, experts say that the percentage of COVID-19 cases that will cause death in nursing homes has declined from 21% to 18%. There is still a great deal of concern, however, about states that are seeing an increase in cases.
Global Crisis in Nursing Homes Due to Lack of Equipment and Care
A decline in the number of COVID-19 related deaths is partially attributed to healthcare facilities learning how to manage the disease. Unfortunately, long-term care facilities have been on the sidelines since the pandemic began, not receiving the same amount of equipment and care that hospitals and clinics have received. This has created a tremendous gap in their ability to care for residents.
Efforts to help nursing homes have also been delayed, with many efforts not starting until July. Here in the U.S., the federal government announced that nursing homes would receive rapid test kits in mid-July – months after the pandemic began. Only 1,500 facilities have received those tests so far. Throughout the pandemic, nursing homes have consistently struggled with a lack of access to personal protective equipment (PPE), sanitation tools and tests.
Facilities in the U.S. are also struggling to pay for tests, which can cost up to $100 per test. If a nursing home has 300 residents, the facility has to find $30,000 in funds to supply one test per resident. Federal support offered through coronavirus relief funding in March has all but dried out, leaving many facilities in a difficult position.
Senior policy attorney at the Center for Medicare Advocacy and advocate Toby Edelman says,
“Nursing facilities do not have enough staff, tests, and personal protective equipment,” adding that as a result, they “remain dangerous places, for residents and workers alike.”
Global Crisis Extends Far Beyond the U.S.
U.S. nursing homes are not the only ones struggling during the COVID-19 pandemic. In fact, facilities across the world report alarming COVID-19 response efforts. In Belgium, nursing home staff report similar shortages in PPE and other supplies. Staff members actually wore gowns and masks from Halloween costumes because they had nothing else to protect themselves with.
Nursing home staff also report receiving little help from hospitals and healthcare providers. On several occasions, staff members report being advised to give the patient morphine and “let death come.” Paramedics and hospitals sometimes denied care to patients with coronavirus, even if there were empty beds. Hospitals attempting to avoid being overwhelmed essentially ignored nursing home residents. Now, Belgium has one of the highest COVID-19 death rates, with 5,700 deaths among nursing home residents.
In Italy, a different scene emerged as hospitals were overwhelmed and medical supply shortages caused problems with providing care. Sweden reports that emergency doctors are turning away elderly patients. In Britain, elderly patients with COVID-19 were sent back to nursing homes, rather than being treated in the hospital. In Spain, prosecutors are investigating instances where residents were abandoned to die.
What’s Next for U.S. Nursing Homes?
What all of this information highlights is the global crisis that continues to plague our nursing homes. The crisis is not COVID-19, but rather an ongoing trend of ignoring these facilities and excluding them from preparedness plans. Public health officials across the world continue to allow this lapse of preparedness to claim lives. It is, quite simply, unacceptable.
Here in the U.S., the number of cases and deaths among nursing home residents is alarming. Sadly, there doesn’t seem to be an end in sight.
Here in the U.S., officials are offering incentives for nursing homes who perform well on their control and management of COVID-19 infections. Distribution of $5 billion in funds through the CARES Act will be based on performance. Thomas Engels, Administrator of the Health Resources and Services Administration (HRSA) says,
“We anticipate that linking payment to performance will be an effective means of holding nursing homes accountable, stimulating innovation, and encouraging them to reach beyond their own walls for infection control expertise and support.”
In addition to performance-based funding, the Department of Health and Human Services (HHS) is also creating a new Quality Roadmap that will focus on transparency, collaboration and accountability. Funding is expected to begin in Mid-August, and it is unclear when the Quality Roadmap will be released.
In the meantime, facilities continue to struggle with outbreaks, staffing shortages and limited access to equipment and supplies.
Sources:
- https://data.cms.gov/stories/s/COVID-19-Nursing-Home-Data/bkwz-xpvg/
- https://abcnews.go.com/US/coronavirus-fatalities-decline-nationwide-viral-deaths-persist-americas/story?id=72271389
- https://www.nytimes.com/2020/08/08/world/europe/coronavirus-nursing-homes-elderly.html
- https://www.hhs.gov/about/news/2020/08/07/hhs-announces-allocations-of-cares-act-provider-relief-fund-for-nursing-homes.html


